We’re ready to get started, are you?
Get in touch and we can connect you with the right people.

Profitably managing an insurance product in the healthcare industry is highly competitive with customers shopping around for the best product at a lowest premium possible. With many product variations and little differentiation between product offerings, it is challenging for insurance companies to retain customers. The ongoing financial crisis and market meltdown adds to this daunting challenge. Experts agree that in the current market scenario, insurance companies have an ever increasing need to optimize and create a simplified product portfolio they can offer and increase their operational efficiency to stay competitive for consumer’s business. An insurer will require dynamic product life cycle management models designed to quickly take advantage of fluctuating market and customer demands. The practice of applying such models to develop and maintain an appropriate balance of products and options in the insurer market’s health product portfolio is termed as Portfolio Management. Successfully managing the product portfolio depends on the availability of the right customer, membership, and benefits information delivered at the right time to make the right management decisions. Understanding how this practice affects an insurer is critical to improving sales, attaining service excellence, and eventually creating a simplified customer experience.
By applying suitable techniques, an organization can balance pricing discipline with membership growth objectives and offer better positioning of the right products and pricing against competition on a targeted sub-segment and geographic basis so as to best package combinations of benefit design, network breadth, access, freedom of choice, care management, wellness and more at the lowest possible price. Effective management of the portfolio of products shows return in the form of improved membership retention, increased sales and profitability, ability to price correctly, tighter control on administrative overhead and enhanced ability to anticipate and introduce new options quickly.
This document describes how a major health care provider applied the product analytics model to optimize the product portfolio strategy and improve business performance within the Portfolio Management practice.
In large healthcare organizations whose footprint spans independent regional markets, the product management practice can be isolated and fragmented across regions. In analyzing the current state of their product portfolio management approach, a major healthcare insurance provider’s product management team discovered complex and disparate processes and product portfolios across the organization. The sheer complexity of the product portfolio was mind-boggling to the management team. This complexity can be attributed because of diverging approaches, mergers and acquisitions, varying data points and lack of process discipline across states and markets. In order to support a vision of optimal product performance where the attributes, pricing and profitability of each product complement the other products in the local market portfolio, the organization decided on implementing an analytic solution to support efficient and consistent evaluation of product performance.
Previously, the healthcare insurance provider relied on numerous stand-alone reports that were pieced together with product information compiled from the many regional data sources. Statisticians and actuaries performed data analysis and mining to find pieces of information that they hoped would prove useful. The product managers would depend on internal data analysts for requests involving consolidating product and membership information and the response time was limiting – at times up to a few weeks. This disorganized and inconsistent product information resulted in ineffective and time-lapsed decision making.
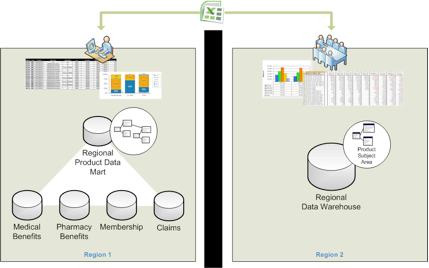
A central data repository of product and membership information is a crucial component in a service-based insurance because it eliminates unnecessary and underutilized products and make the product portfolio simpler to administer and easier to communicate to the customers. Having that information in a single repository and available for analysis and distribution across the enterprise also permits the Product Management team to enable cross-state and cross-segment comparisons, a repeatable data processing framework would need to be implemented that allowed standardized definitions and hierarchies to be layered over disparate data across the various regions into a shared model. In addition, a common access layer would be needed to ensure all regions having access to the same tools and reports. The necessity of a shared common model also introduces the challenge of establishing a strong data governance function responsible for establishing a common product data “language” across the regional product managers.
Because of the enormity of the data and process challenge, the effort to build such a framework had never been attempted before. However the pressing demand for greater efficiency in reacting to competition and to solidify customer retention drove the provider to invest in maturing the supporting data infrastructure surrounding the portfolio management business processes.
Classic, was tasked with assisting the insurer’s project team in architecting and implementing the solution. The solution framework covered fulfilling core data needs of the product management team to support near-term product analysis using regularly refreshed centrally hosted product data for reporting and analysis fronted with reporting and analysis tools. The primary goal of the solution was to develop an analytical, automated product lifecycle management process for monitoring product and portfolio health that supports ongoing analysis, decision making, actions to support strategy and to maximize growth and profitability.
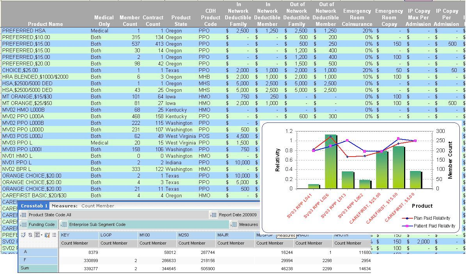
The Classic architected solution was designed and implemented to allow product managers access to an analytical model that supports efficient and consistent evaluation of product performance. Some of the critical data presentation areas addressed which were not previously available directly included:
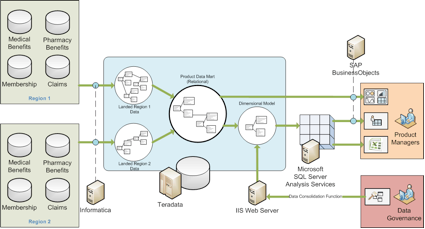
The ad-hoc reporting functionality was realized by leveraging an OLAP cube, built on SQL Server Analysis Services, which provided detailed information on commercial products at a benefit attribute level for both medical and pharmacy products. The reporting, alerting and dashboarding capability was delivered through the corporate standard Business Intelligence tool suite, SAP BusinessObjects.
To feed a common access interface, Classic designed a central data repository that consolidated all product benefit, membership and claims information with a means to map region specific data domains to a shared common data definition. The following technologies were used to create the application:
The data normalization framework was designed and built using a custom built web based metadata-driven application which allowed custom attribute definitions and hierarchies and allowed users to map region specific attributes to the standardized custom definitions.
An ETL solution with a stable, timely, maintainable and extensible framework for converging disparate data sources was built on Teradata’s powerful parallel-architecture platform. The initial phased rollout of the product data mart sources the product benefit data for two regions and then standardizes, integrates and loads the data into about 30 tables.
The data is accessible to the user community via SAP BusinessObjects Web Intelligence and Voyager tools as well as through the Microsoft Excel. SAP BusinessObjects Web Intelligence provides access to seven standard reports and SQL Server Analysis Services cube, accessible via the Voyager tool and Excel, provides detailed analysis of insurer’s commercial products at a benefit attribute level for both medical and pharmacy products.
Below are a few testimonials from the Product Management team:
“This work is one of the key deliverables for the Portfolio Management track of the Product Simplification initiative, and takes to the next level the Portfolio Management Framework, which was rolled out to the Commercial Product team earlier in 2009. The Product Analytics tools provide the Commercial Product Management team with enrollment and product performance data at the benefit design level (medical and pharmacy), equipping the team to more effectively manage our standard product portfolios and recommend data-driven benefit and portfolio actions.”
Director, Product Planning and Reporting
“This is a very important accomplishment.”
SVP Chief Marketing and Product, Commercial Business Unit
The market is always changing and is inevitable. Insurance companies are always examining ways to operate more efficiently, which is essential to allow them to invest for the longer term and to innovate for the benefit of their customers and members. It has become increasingly clear that the most successful insurers will be the ones that can offer innovative, differentiating products that appeal to increasingly savvy and technologically empowered customers. By simplifying and standardizing their product portfolio, insurers can increase customers’ understanding of the various product offerings, improve customers’ overall experience and minimize ongoing operational expenses.
Standardization is the key to a successful enterprise. Using integrated analytic engines, an insurer can not only simplify and optimize their product portfolio but can also bridge the gap between health, care and value.
Get in touch and we can connect you with the right people.